How To Test Everyone — Thru Poop
Three studies on detecting COVID-19 in wastewater

How do you test everyone for COVID-19, all the time, and anonymously? Well, everybody poops.
Three recent studies have tested entire populations in Amsterdam, Paris, and Massachusetts for COVID-19. These cheap, simple wastewater tests have shown when the virus started spreading, when it started accelerating, and when regular testing was missing something.
Your poop is anonymized in the flush, so it cannot tell if you have COVID, it can tell public health officials when and where an outbreak is starting, so they can deploy scarce PCR testing strategically. In fact, wastewater testing could be used for future epidemics, for viruses and bacteria we haven’t even heard of yet. All you need is a fragment of the target RNA and 250ml of murky water. It’s a big data dump that we’re literally just sitting on.
Here’s how it works.
Wastewater Monitoring

If a virus is in your body, it’s likely coming out of your butt. Even diluted, a simple test can find RNA fragments miles downstream in wastewater. This technique has been used for poliovirus, Aichi virus, and measuring antibiotic resistance. You can even guess how much cocaine a town is doing.
Wastewater monitoring works for COVID-19 as well.
Amsterdam
The basic method is to collect a bit of wastewater over a 24 period and just do a CTRL-F for some RNA fragments.
In February, Gertjan Medem et al (KWR Water Research Institute) did just this at eight locations in Amsterdam. They transported 250ml samples on ice and tested them the same day. This what they found:
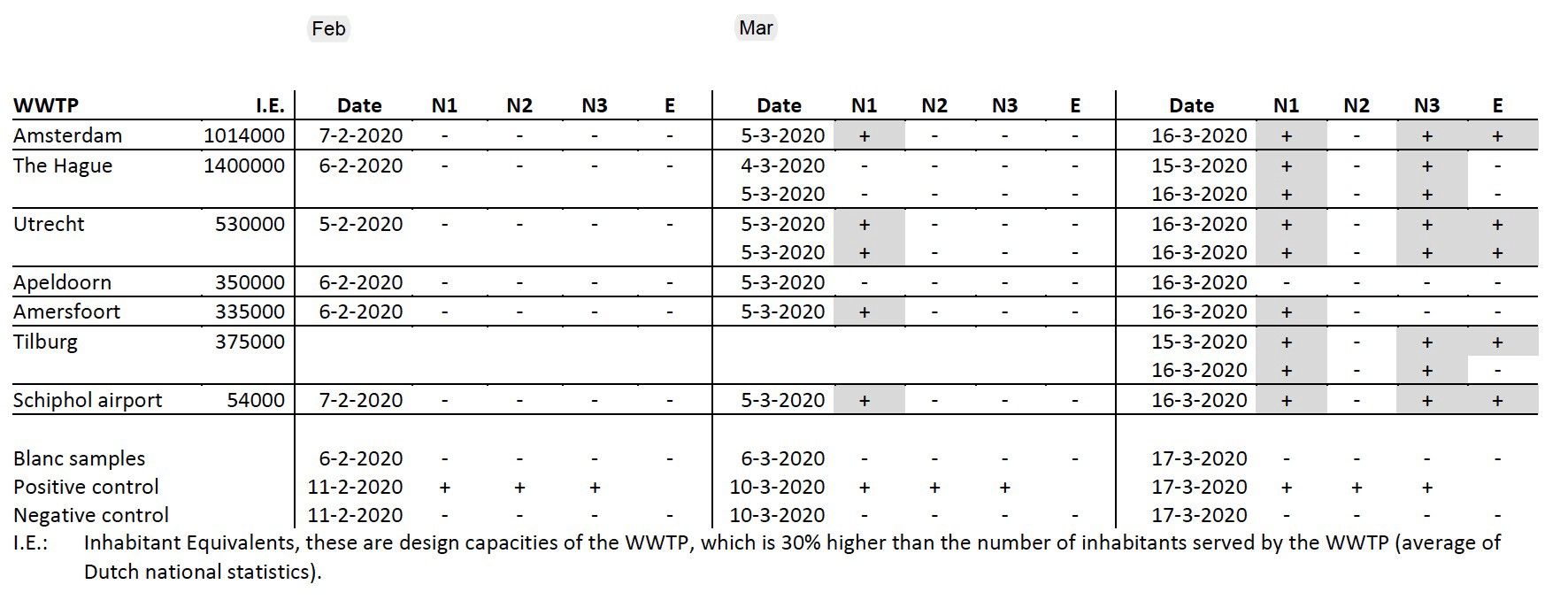
To make this easier to read, just look at the three main columns. They mark three tests, one before the virus hit, and two after. In February (before) there were no hits on any of the RNA fragments (N1–E).
After the first reported case on February 27th, however, they got a hit. The Ctrl-F they were running for ‘GACCCCAAAATCAGCGAAAT’ (N1) came up positive. Later they got more hits, for different bits of code. The virus was in the wastewater, and it was easily and cheaply detectable, even at low amounts.
Since the wastewater was collected at specific plants, this method also told them roughly where the infections were. Not where the exact toilet was, but the general vicinity of the butt. This has a lot of potential. You can’t use it to test/trace/isolate, but it can tell health officers roughly where to start.
It’s a powerful collection system, spread across an entire population. Everyone was giving samples every day, all anonymized in the flush.
As the authors said:
This is the first report of detection of SARS-CoV-2 in sewage. The detection of the virus in sewage, even when the COVID-19 prevalence is low, indicates that sewage surveillance could be a sensitive tool to monitor the circulation of the virus in the population.(Presence of SARS-Coronavirus-2 in sewage)
The authors Gertjan, Leo, Goffe, Ronald, and Anke showed that this method could work, but the next question was velocity. Beyond a yes or no, could this method tell us how fast the virus was accelerating?
For that answer, we’ll go to Paris.
Paris
In March, Sebastien Wurtzer et al (Eau de Paris and the Sorbonne) started testing samples from three wastewater treatment plants around Paris. You can see the results in the graph below:
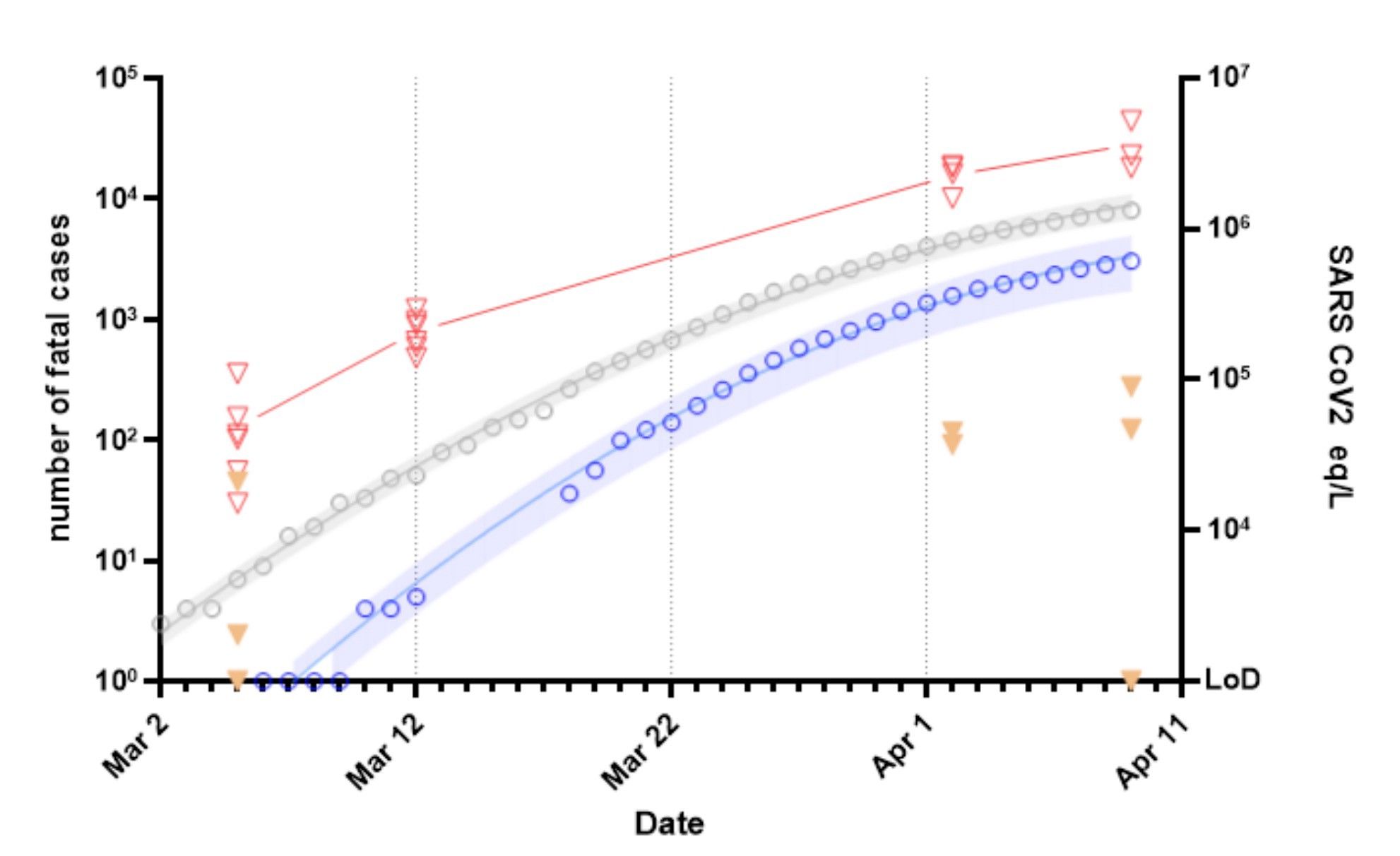
The red line roughly tracks (and leads) the accelerating death count in Paris (blue). By doing one basic test on March 5th, they knew that COVID-19 was in the population, and by continuing to monitor they could see the velocity, later sadly confirmed with deaths.
Our study demonstrates that the contamination of wastewater and the detection of viral genome occurred before the beginning of the exponential growth of the epidemic. (Time course quantitative detection of SARS-CoV-2 in Parisian wastewaters)
In short, if you were watching the stools, you could see it coming. This is the big question we’re asking here. Not how do we test better, but how do we use tests to stop epidemics from happening at all.
The tests we have now are PCR, which is expensive and requires testing people one by one, or ‘rapid’ blood-testing, which only gives a hit weeks after you’ve been infected. We need something else. Something cheaper, faster, and better.
Wastewater sampling offers another approach. Instead of testing individuals, we test an entire population. Then we use that information to narrow down with the usual tools. This sort of general surveillance has a lot of potential. In fact, if we store samples we could reach the epidemiological holy grail as well — finding out where a virus started.
This would notably argue for the long-time conservation of wastewater samples in dedicated local wastewater-bank, which would allow a retrospective investigation of pathogens circulation.
Additionally, wastewater survey may provide an alternative and possibly early tool to detect pathogens in populations when investigations in humans is difficult for logistic, ethical or economic reasons. (Time course quantitative detection of SARS-CoV-2 in Parisian wastewaters)
The authors Sebastien, Vincent, Jean-Marie, and Laurent were able to show not only that an epidemic was happening in Paris, but also that shit was about to hit the fan.
The next question is whether this method can tell us more than our current approach.
For that, we’ll go to Massachusetts.
Massachusetts
Like their compatriots in Europe, Wu et al (MIT) found viral RNA in wastewater. That much is known. However, the title of their paper was ‘higher than expected’. Tracking wastewater was telling them something conventional testing wasn’t.
Viral titers observed were significantly higher than expected based on clinically confirmed cases in Massachusetts as of March 25. The reason for the discrepancy is not yet clear, and until further experiments are complete, these data do not necessarily indicate that clinical estimates are incorrect. (SARS-CoV-2 titers in wastewater are higher than expected)
To reach this observation, the authors backtracked from the weight of an average poop (200g), how many people were dropping a daily deuce (2.3 million), and how much it was diluted (1.36 billion liters). Further research is required on how much viral load is coming out of the butt and how it dilutes, but it’s all very promising.
The implications of this research are that WBE can be leveraged to detect population-level prevalence of SARS-CoV-2 in cities across the world.
These data may help inform decisions surrounding the advancement or scaleback of social distancing and quarantine efforts based on wastewater catchment-level estimations of prevalence.
Additionally, wastewater collection at the municipal or community level may allow for more granular detection of SARS-CoV-2 in cities with lower COVID-19 disease burden, thereby functioning as an early warning system to help preemptively enact public health measures prior to the widespread onset of disease. (ibid)
Fuqing, Amy, Jianbo, Xiaoqiong, Wei Lin, Kathryn — deep breath — William, Mariana, Newsha, Noriko, Claire, Katya, Timothy, Peter, Janelle, and Eric reinforced the earlier conclusions, and also showed that this data might tell us more than we already know. At a population level, wastewater information might be good enough to release lockdowns or catch early epidemics before they start.
They rightly pointed out the need for much more research, and this should be done while people (especially in the US) are shitting out samples every day. We should be using those samples to calibrate this method and make it into a more precise tool. If we can do that, it’s a real asset to global public health.
The Power Of Poop
The holy grail of pandemics is not having them at all. The holy grail is catching a virus very early and squashing it. We did that (painfully) with SARS and MERS, but the asymptomatic nature of COVID-19 has completely evaded our usual testing regime.
Individuals only show up for a test when they’re symptomatic, and even then we don’t have enough tests. This is usually days or weeks later, and some people never show symptoms at all. They’re still shedding virus the whole time.
We need a way of catching that virus they’re shedding, and the daily stool sample we all give is the simplest route.
The appeal of wastewater testing is that any scientist could take an RNA fragment, walk over to a wastewater plant, and CTRL-F it in a PCR machine. This would tell with a high sensitivity whether the virus was circulating at all (like in Amsterdam), how fast it was spreading (like in Paris), and whether we were missing something big (like in Massachusetts).
In fact, this level of surveillance could just be built-in. This level of checks can just become part of our sanitation system. Sanitation, after all, means health.
Samples could be constantly tested for known pathogens and stored if we need to backtrack. The minute an epidemic pops up in Hong Kong or Kansas or wherever, we can CTRL-F for that RNA and see if we get a hit.
We’re literally sitting on a giant data dump here — anonymized, geo-tagged, and used by the entire global population. Not everyone uses Google or Facebook, but everybody poops. There’s a lot more research to be done, but hey. Let’s have a look.
Notes
I have cited three preprint papers in this article. They are not yet peer-reviewed, and I am not a peer. I highly recommend reading the articles yourselves (they’re short) and please understand that this science is very much a work in progress.
Amsterdam
Presence of SARS-Coronavirus-2 in sewage
Gertjan Medema, Leo Heijnen, Goffe Elsinga, Ronald Italiaander, Anke Brouwer
doi: https://doi.org/10.1101/2020.03.29.20045880
Paris
Time course quantitative detection of SARS-CoV-2 in Parisian wastewaters correlates with COVID-19 confirmed cases
Sebastien Wurtzer, Vincent Marechal, Jean-Marie Mouchel, Laurent Moulin
doi: https://doi.org/10.1101/2020.04.12.20062679
Massachusetts
SARS-CoV-2 titers in wastewater are higher than expected from clinically confirmed cases
Fuqing Wu, Amy Xiao, Jianbo Zhang, Xiaoqiong Gu, Wei Lin Lee, Kathryn Kauffman, William Hanage, Mariana Matus, Newsha Ghaeli, Noriko Endo, Claire Duvallet, Katya Moniz, Timothy Erickson, Peter Chai, Janelle Thompson, Eric Alm.
doi: https://doi.org/10.1101/2020.04.05.20051540
Images for this post are based on elements from freepik.com.